VAERS and Myocarditis
Digging into VAERS and its role in vaccine safety as well as recent studies regarding the risk of post-vaccination myocarditis
VAERS
If you’ve been paying attention during the last two years, you’ll absolutely have heard of VAERS. The Vaccine Adverse Event Reporting System is a pharmacovigilance system meant to detect vaccine safety risk signals not discovered during initial clinical trials.
You’ll likely also have seen graphs like this at one point or another:
At first glance it might appear that this staggering number of deaths absolutely confirms the danger of these vaccines. Generally, you'll come across two common arguments against using the data:
It is unreliable because anyone can submit a report. What often goes unsaid is that falsification of an adverse event by an individual or a physician is punishable by federal fines, imprisonment, or loss of medical license.
Reports do not prove causation (ie: a death reported to VAERS is not necessarily the result of the vaccine). This is true, VAERS data is correlative only.
As always, the truth is more complicated than meets the eye. What is abundantly clear, however, is that it is incumbent on our public health agencies to investigate these correlations and determine if causal relationships exist. Refusal of these agencies to infer causality renders the entire purpose of pharmacovigilance useless1.
“…I have been disappointed to find that corporations who develop vaccines and have a vested interests in the profitability of vaccines, and regulatory agency members who, it turns out, also have financial vested interests in vaccines, routinely partake in science-like activities.” - James Lyons-Weiler
You might ask, has a vaccine ever been suspended based on reports in pharmacovigilance systems like VAERS? The answer is yes. In 1999, the CDC used VAERS data to suspend the use of the rotavirus vaccine in infants2.
Common sense would lead us to believe that similar analysis of VAERS data by our public health agencies would be on-going but, for the COVID-19 vaccines, we've largely had to rely on independent analysis for any answers at all.
In June 2021, an analysis of 250 out of the 1644 deaths was released by McLachlan et al., revealing that the vaccine could not be ruled as the cause of death in 86% of cases3. We have since surpassed 22,000 reported deaths,with no such follow-ups to this study conducted by either independents or public health agencies.
In September 2021, Josh Guetzkow came out with a report comparing adverse events between the flu and COVID-19 vaccines. Using the CDC’s own analysis methods, the proportional reporting ratios revealed an increased risk of serious adverse events (28x), death (91x), and myocardial infarction (126x)4.
Both of these reports reveal particularly concerning information regarding the COVID-19 vaccines, but neither came from the agencies who are actually responsible for the safety of medical products. It raises the question, what else has been missed?
Myocarditis
Causal links between myocarditis and COVID-19 vaccines have existed for awhile. However, it hasn’t been until recently that they’ve been propelled into the spotlight, thanks in part to the recent Rogan/Malone podcast. We should not have to rely on the Joe Rogan Experience to ring this alarm bell, yet here we are.
A common claim you’ll undoubtedly hear about post-vaccination myocarditis is that it is both rare and mild. As with many aspects of the vaccine and this pandemic, these statements have quickly been turned on their head.
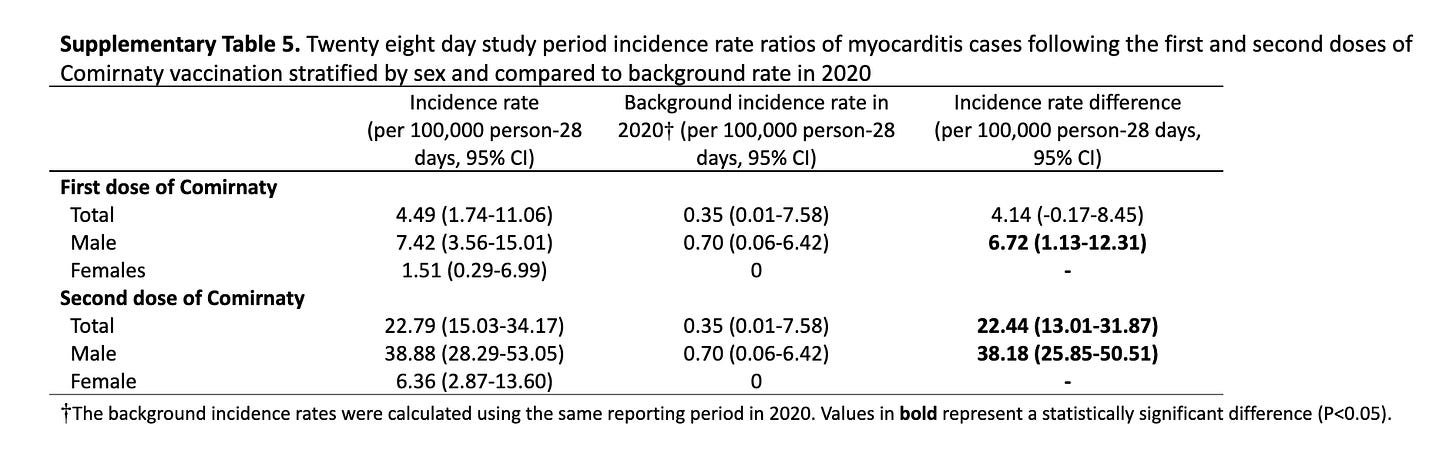
Recent studies have reported rates of post-vaccination myocarditis ranging from 38-54 / 100k in males aged 12-24 after the second dose5,6,7.
The drive the point home, these rates were almost 10x greater than what the CDC expected (1.9-8.3 cases / 100k)8.
Were these the rates experts were using to justify their claims of the rareness of the adverse event? It is difficult to tell, as they did not cite a source when they made the claim.
If that were the extent of the evidence it would be bad enough, but there is more.
Patone et al. published two articles showing a higher risk of myocarditis from vaccination than natural infection in males under 40 years of age9,10.
Clearly, the experts couldn’t have been further from the truth when they spoke of the rarity of this condition.
The last and more concerning question then is how wrong were the experts about the mildness claim? The truth is, we really don’t know. A large part of mortality from classical forms of myocarditis comes years down the road.
What we do know is that this is a potentially serious adverse event and that long-term outcomes are currently unknown and require more study11,12,13.
“…long-term risks associated with postvaccination myocarditis remain unknown. Larger studies with longer follow-up are needed to inform recommendations for COVID-19 vaccination in this population.”
“Although most of these events were mild, some of them, such as myocarditis, could be potentially serious.”
“…long-term implications, and mechanism of this myocardial injury needs to be studied further, especially as vaccination efforts are rolled out to younger children.”
In just a few short months the conversation on post-vaccination myocarditis started at mild and rare but has quickly morphed into potentially more common in certain age groups than natural infection and with unknown long-term effects. A vastly different statement, one that should cause people to pay attention, especially as we administer these vaccines to our children.
What is the cause of this? Why is it happening predominantly in males aged 12-24? Why after the second dose? Our questions have gone unanswered for too long, and we deserve the answers.
#DemandTheTruth
https://www.publichealthpolicyjournal.com/_files/ugd/adf864_4588b37931024c5d98e35a84acf8069a.pdf
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4843a5.htm
https://www.researchgate.net/publication/352837543_Analysis_of_COVID-19_vaccine_death_reports_from_the_Vaccine_Adverse_Events_Reporting_System_VAERS_Database_Interim_Results_and_Analysis
https://drive.google.com/file/d/1IAzK4a58a7M4ajHKOpqe-9KD9PdYAVpr
https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciab989/6445179
https://www.medrxiv.org/content/10.1101/2021.12.02.21267156v1
https://www.medrxiv.org/content/10.1101/2021.12.21.21268209v1
https://www.fda.gov/media/150054/download
https://www.nature.com/articles/s41591-021-01630-0
https://www.medrxiv.org/content/10.1101/2021.12.23.21268276v1.full-text
https://jamanetwork.com/journals/jamacardiology/fullarticle/2783052
https://www.nejm.org/doi/10.1056/NEJMoa2110475
https://publications.aap.org/pediatrics/article/148/5/e2021053427/181357